7 Neonatal Jaundice
7.1 Introduction
Jaundice is the yellowish discoloration of the skin, eyes and mucous membranes, caused by a pigment called bilirubin in the blood. Out of 10 term and 10 preterm newborns, 6 and 8 will develop jaundice respectively, all in the 1st couple of weeks of life. Universally accepted as one of the commonest causes of admission and readmission in the first month of life. At Komfo Anokye Teaching Hospital Mother Baby Unit, monthly admissions average between 300 and 400 and about 15 to 25% of all these admissions are cases of neonatal jaundice. Whereas the developed world describes kernicterus as a rare condition, unfortunately, the same cannot be said for us in developing countries. On average, cases of severe Neonatal Jaundice have ranged from 2.2% to 30.8% of all jaundice cases, with the monthly mortality ranging from 2.8% to 15.2%(REFERENCE). Remember, kernicterus is the only preventable cause of cerebral palsy!
7.2 Bilirubin metabolism
Humans continuously form bilirubin and the liver is the main organ responsible for the metabolism of bilirubin. For every gram of haemoglobin, 35mg of bilirubin is produced. The bilirubin is conjugated by the UGT enzyme, making it water-soluble, which is then released into the bile before being excreted in the stool (and urine). It can also be broken down in the intestine by bacterial enzymes like E. coli. However, at birth, the newborn has several challenges. The liver is immature, and the levels of bilirubin uridine diphosphate glucuronosyltransferase (bilirubin-UGT) enzyme are low. Newborns have β-glucuronidase in the intestinal mucosa/brush border, which deconjugates the conjugated bilirubin found in the meconium. The unconjugated bilirubin can now be reabsorbed through the intestinal wall and recycled back into the circulation. This process is known as the “enterohepatic circulation of bilirubin”. The gut is sterile and, subsequently, infants have far fewer bacteria in the gut, and so very little, if any, bilirubin is reduced to urobilin and stercobilin.
Specifically in newborns, more bilirubin is produced, on account of the short life span of Red Blood Cells and high Hemoglobin levels. The liver is immature. They also have fewer bacteria and low intestinal enzymatic activity in the intestine
7.3 Types of bilirubin
There are two types:
7.3.1 Conjugated (Direct) Bilirubin
This is water soluble, excreted in the urine and stool, and not toxic to the brain. However, high amounts could indicate underlying liver disease or injury.
7.3.2 Unconjugated (Indirect) Bilirubin
This is lipid soluble, can cross the blood-brain barrier and is toxic in high amounts to the brain.
In very high concentrations, unconjugated bilirubin, which is lipid-soluble, is toxic to the developing brain. Once it crosses the blood-brain barrier, it binds to brain tissue and deposits in the developing brain. Since this is an irreversible process, it leads to long-term neurological issues and even death.
7.4 Types of Jaundice
There are two main types of jaundice:
- Physiological jaundice and
- Pathological jaundice.
There are three main mechanisms for jaundice:
- Increased bilirubin production
- Decreased bilirubin clearance and
- Increased enterohepatic circulation.
7.4.1 Physiological jaundice
7.4.1.1 Increased bilirubin production
in term newborn infants, bilirubin production is 2 to 3 times higher than in adults. This occurs because newborns have more RBCs and fetal RBCs have a shorter life span than those in adults. Unfortunately, the liver being immature, cannot conjugate and excrete all the bilirubin from the breakdown of all the excess RBCs, thereby resulting in spillover of bilirubin into the blood.
7.4.1.2 Bilirubin clearance or excretion
This is decreased in newborns, mainly due to the low levels of the UGT enzyme in the liver. UGT activity in term infants at day 7 of age is approximately 1% of that of the adult liver and does not reach adult levels until about 14 weeks of age.
7.4.1.3 Enterohepatic circulation
The presence of the ß-glucuronidase results in an increase in the enterohepatic circulation of bilirubin, further increasing the bilirubin load in the infant. This is a diagnosis of exclusion
7.4.2 Pathological jaundice
7.4.2.1 Definition
Neonatal jaundice is said to be pathologic if:
- Jaundice in the 1st 24 - 48 hours of life.
- Rate of SB rise > 0.5 mg/dL (8.5µmol/L) per hour
- Jaundice all over the body (including palms & soles)
- Presence of a danger sign
- History of previous siblings having had jaundice at birth
- Jaundice in a term newborn after 2 weeks of age or in a preterm infant after 3 weeks of age
- Direct (conjugated) bilirubin concentration > 20% of the total
It can be caused by certain pathologic conditions or exaggeration of the mechanisms responsible for physiologic neonatal jaundice. Identification of what is causing the jaundice is useful in guiding management, including counselling of the parents and what to expect for the next pregnancy. Most common cause is increased bilirubin production due to haemolytic disease processes that include the following:
- Isoimmune-mediated haemolysis (e.g., ABO or Rhesus D incompatibility)
- Erythrocyte enzymatic defects, e.g. G6PD deficiency
- Sepsis, especially Urinary Tract Infection
- Polycythaemia
- Birth Injuries resulting in sequestration of blood within a closed space, e.g. cephalohematoma, subgaleal bleed.
7.4.2.2 ABO incompatibility
This is one of the most common causes of isoimmune hemolytic disease during the neonatal period. Infants with blood group A or B, carried by blood group O mother, will have a positive antibody because of maternal anti-A or anti-B transfer into the fetal circulation.
7.4.2.3 Rhesus Incompatibility
Rh incompatibility can occur when an Rh-negative pregnant mother is exposed to Rh-positive fetal red blood cells secondary to feto-maternal haemorrhage during pregnancy/delivery. As a result, the mother’s blood gets exposed to the fetal circulation and sensitization occurs leading to maternal antibody production against the foreign Rh antigen. Once produced, maternal Rh (IgG) antibodies may cross freely from the placenta to the fetal circulation, where they form antigen-antibody complexes with Rh- positive fetal RBCs and eventually are destroyed, resulting in a fetal alloimmune-induced hemolytic anaemia and jaundice. The first pregnancy is usually not affected, but more antibodies are produced with each pregnancy making the jaundice worse with each pregnancy.
7.4.2.4 Decreased clearance
Inherited defects in the gene that encodes the UGT liver enzyme (eg, Gilbert Syndrome), decrease bilirubin conjugation (eg Crigglar Najjar). In physiological jaundice, the levels are naturally low, but here, in addition to the low levels the UGT enzyme is either defective, absent or has a reduced function. This reduces hepatic bilirubin metabolism and its clearance thereby increasing the total serum unconjugated bilirubin levels.
7.4.2.5 Increased enterohepatic circulation
The major causes are
- Breastfeeding jaundice
- Breast milk jaundice
- Impaired intestinal motility is caused by functional or anatomic obstruction.
- Congenital hypothyroidism also causes increased enterohepatic circulation on account of reduced gut motility.
7.5 Assessing for Neonatal Jaundice
- Baby should be assessed in natural daylight
- Look for yellow eyes & skin, check the white part of the eyes only if the baby opens the eyes voluntarily.
- You may blanch the skin on the bridge of the nose or the palms/soles of the feet if they turn yellow…
- Remember that the yellowing spreads from head to toe…
- Do not rely on visual inspection alone to estimate the bilirubin level in a baby with jaundice!!! It can be very subjective!!
7.6 Clinical features
The clinical features of neonatal jaundice may include:
- Baby looks yellow! The yellowness appears cephalocaudal.
- May not be as active as he/she used to be
- Lethargic/hypotonic
- Weak cry, irritable
- Poor feeding
- High-pitched cry / poor cry
- Seizures
- Arching of the neck/back
Thus to evaluate a child with jaundice we:
- Determine birth weight, gestation and postnatal age (in hours)
- Assess clinical condition (well or ill)
- Degree of jaundice (visual inspection, SBR etc)
- Look for evidence of kernicterus / BIND
7.7 Management
The general principle of treatment includes
- Encourage frequent exclusive breastfeeding.
- Start Intravenous fluids only when there are signs of dehydration
- Watch out for danger signs
- Pathologic Neonatal jaundice is treated with
- Phototherapy
- Exchange Blood Transfusion (EBT)
- Antibiotics
Be interested in the cause as this will serve as a guide in the management of the baby and direct your counselling as well as impact on subsequent pregnancies Loads of information in the maternal and child health record book, Gravidity and Parity, G6PD status, maternal Blood group & Rhesus status etc
7.7.1 Investigations
This should include but not be restricted to
- Serum Bilirubin (conjugated, unconjugated and total)
- Full Blood Count
- G6PD screening
- Blood Culture & Sensitivity
- Baby’s blood group (only necessary if mother’s blood group is O)
- Others include Direct Coomb’s test, Urine C & S etc
7.7.2 Phototherapy
Phototherapy is the use of visible light to treat high levels of serum bilirubin in the newborn.

The dose of phototherapy is a key factor in how quickly it works. The dose in turn is determined by:
- The wavelength of the light
- The intensity of the light (irradiance)
- The distance between the light and the baby
- The body’s surface area is exposed to the light.
Effective phototherapy lowers serum bilirubin levels by converting the lipid-soluble bilirubin into water-soluble forms that can easily be excreted in the stool and urine Phototherapy also prevents the need for an Exchange Blood Transfusion and prevents bilirubin from depositing in the brain. The breakdown of bilirubin begins almost instantaneously when the skin is exposed to light, hence, phototherapy should be started as early as possible.
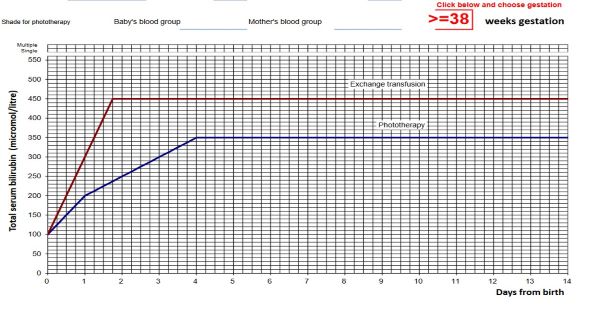
In initiating phototherapy, always note the time the baby’s SBR sample is being taken and estimate the age in hours up until that time. Interpret bilirubin levels according to the baby’s postnatal age in hours and manage the bilirubin levels according to the threshold table Start phototherapy if the SBR plots on or above the line appropriate for age (in hours) and gestational age If the SBR plots just underneath the line, repeat the SBR after 6 hours or start phototherapy if a repeat is not feasible. Repeat the SBR at least 24 to 48 hours after initiation of phototherapy. Discontinue phototherapy when the SBR plots below the line.
The side effects of phototherapy include:
- Increase insensible water loss
- Loose stools
- Skin rash
- Bronze baby syndrome
- Hypo- or Hyperthermia
- Interruption of mother-baby bonding
7.7.3 Sunlight Therapy
Works for physiological jaundice, however, one can never tell by looking at a baby what kind of jaundice a baby has Err on the side of caution, at least always have the SBR checked first Remember prolonged exposure to UV rays can be harmful to the developing skin Baby cannot be put in the light for more than 30 minutes in a day Even most of the available literature and studies that recommend sunlight still advice that if the jaundice is severe, the baby must be managed in the hospital!! A serum bilirubin high enough to warrant treatment should be managed in the hospital.
7.7.4 Exchange Blood Transfusion
Provides a means of rapid reduction of circulating bilirubin in the blood. Involves manual removal of the baby’s blood and simultaneously replacing it with compatible donor blood.

In addition to reducing bilirubin levels, EBT removes partially hemolyzed RBCs, RBCs coated with antibodies and circulating immunoglobulins.
Complications of exchange blood transfusion include:
- Cardiac & respiratory disorders
- Shock due to bleeding or inadequate replacement of blood infection
- Catheter-related complications
- Changes in the composition of the blood (high or low potassium, low calcium, low glucose, changes in pH)
- Thrombocytopenia
- And the rare but serious complications of air embolism, portal hypertension, and necrotizing enterocolitis.
7.7.5 Intravenous Immunoglobins
Treatment with intravenous immunoglobulin (IVIG) has been suggested as an alternative therapy to Exchange Blood Transfusion for isoimmune hemolytic jaundice to reduce the need for Exchange Blood Transfusion and duration of phototherapy and hospitalization in isoimmune hemolytic disease of the newborn. It has been proposed that IVIG blocks the binding of the antibody to the antigen. With this blockade, hemolysis no longer occurs.
7.8 Long term complications
The effects of bilirubin toxicity include
- Hearing loss
- Cerebral palsy
- Mental retardation
- Dental complications
- Delayed developmental milestones
- Seizure and visual disorders
7.9 Recommendations
- Always err on the side of caution
- An SBR is always more objective
- Look out for danger signs
- As much breastmilk as possible by any means necessary
- Sunlight therapy is not recommended, if the baby is yellow enough for you to want to put him/her under the sun, then the baby needs to be brought to the hospital!