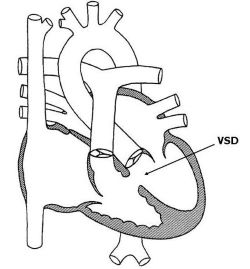
23 Ventricular Septal Defect
23.1 Introduction
This is the most common Congenital Heart Disease (CHD), being seen in about 15-20% of all CHDs. VSD occurs in different anatomical locations. The most common is the peri-membranous. Others are inlet, outlet, muscular and infundibular. They also appear in different shapes and sizes as well.
23.2 Pathophysiology
Typically VSD without the presence of another congenital heart malformation results in a left to right ventricle shunting lesion because of the pressure difference. Thus, a VSD is usually an acyanotic congenital heart lesion. This leads to a volume overload of the pulmonary artery, lungs, left atrium and left ventricle. These chambers subsequently dilated. Pulmonary edema develops from lung congestion leading to signs of heart failure.
Secondly, depending on the size of the defect the pressure in the left ventricle will get transmitted to the right. How much pressure is transmitted depends on the size of the defect with bigger defects transmitting more than smaller ones. This can result in increased right ventricular pressure, and hypertrophy. It also worsens the pulmonary oedema already mentioned above.
Persistent pressure and volume overload cause remodelling of the pulmonary vasculature, resulting in permanent changes and pulmonary hypertension. When the pulmonary pressure rises significantly higher than the systemic pressure, a reversal of the shunt results, leading to decreased oxygen saturation.
23.3 Clinical presentation
The clinical presentation of VSDs is variable and depends on the size and position.
Position: A perimembranous VSD of comparable size may exhibit more signs of heart failure than one that is mid-muscular or apical.
Size: Generally, the sizes of VSDs determine the extent of the volume and pressure overload of the right heart and lungs. Larger ones result in relatively higher pressure and volume. Small VSDs are usually asymptomatic with no volume or pressure overload of the lung, pulmonary artery and right heart. Some volume and pressure overload usually accompanies moderate-sized VSDs. They are thus often accompanied by some heart failure and recurrent lower respiratory infections. Large defects are accompanied by severe volume and pressure overload. They present with persistent heart failure and failure to thrive, exercise intolerance. When longstanding, they often end up with significant pulmonary hypertension.
Newborns with VSD may not have a murmur at birth. This is due to relatively high pulmonary pressure in the first weeks of life. The intensity of the murmur may increase as the pulmonary pressure decreases, usually over 4 weeks. The patient then becomes more symptomatic with a louder pansystolic murmur loudest at the lower left sternal border. Patients with a large defect may present with an apical diastolic rumble. Cyanosis may present in a long-standing large VSD with pulmonary hypertension.
23.4 Investigations
- At the bedside pulse oximetry would likely reveal a normal SpO2 as this is an acyanotic congenital heart disease.
- A chest X-ray could show cardiomegaly with dilatation of the left side of the heart. Increased vascular markings may also be present.
- The electrocardiogram will likely show features of left ventricular dilatation and left atrial enlargement.
- An echocardiogram is diagnostic as it visualises the defect, quantifies the shunt and other chamber sizes, and identifies possible complications.
- Cardiac catheterisation is often done in cases of moderate to large defects. to detect complications such as possibly pulmonary hypertension, and quantify the shunt volume.
23.5 Treatment
Treatment modalities depend on the patient’s age, defect size and location, associated symptoms and complications. Small defects in the very young, without signs of heart failure, can be treated by watchful waiting as some may close spontaneously. Defects accompanied by heart failure symptoms should be treated for heart failure while planning for possible surgical ligation is being done. Large defects are treated the same but with more aggressive heart failure management and urgent surgical therapy. This is because these are often accompanied by a failure to thrive, poor feeding and generally poor health.
Current surgical treatment involves device closure, but some centers such as Ghana still close the defects with an open heart surgery. Also, there are certain circumstances where a device closure cannot be done, thus open heart surgery becomes the only option.
23.6 Prognosis
In many developed countries, the prognosis of VSDs has become excellent with surgical and device treatment. (Jortveit et al. 2016) However, in Ghana, most patients do not realistically have the chance of early surgical correction. Thus the prognosis of VSDs with significant symptoms tends to be poor.
23.7 Differential diagnosis
Differential diagnosis of a ventricular septal defect is mitral regurgitation and tricuspid regurgitation.
23.8 Complications
Notable complications of VSDs include Infective Endocarditis, aortic regurgitation, pulmonary hypertension, left ventricular outflow tract obstruction and growth failure.